Signed in as:
filler@godaddy.com
Signed in as:
filler@godaddy.com
The Short Answer: The scientific process of diagnostic thermal imaging and analysis.
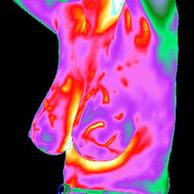
The Long Answer: Medical thermology is the science that derives diagnostic indications from highly detailed and sensitive infrared images of the human body. Medical thermology is sometimes referred to as digital infrared imaging, medical infrared imaging, infrared mammography or tele-thermology and involves the use high thermal and spatial resolution infrared (thermographic) cameras. Medical thermology is a patho-physiologic discipline that is completely non-contact and involves no form of energy imparted onto or into the body. Medical thermology has established applications in breast oncology, cardiology/vascular medicine, chiropractic, dentistry, neurology, occupational medicine, orthopedics, pain management and veterinary medicine. We specialize in breast and vascular thermology.
The Short Answer: Medical thermology can reveal the abnormal metabolic and blood-flow features that cause changes in the temperature of the skin that are characteristic of certain types of diseases including breast cancer.
The Long Answer: Skin temperature is a result of blood-flow and metabolic activity near the surface of the body. Medical thermology provides a means of evaluating skin temperatures for specific abnormalities in patterns, levels and behaviors that are characteristic of certain disorders and diseases. Medical thermology is completely different from all other forms of diagnostic imaging as it evaluates features of body function (physiology) rather than structure (X-ray, ultrasound or MRI).
The glandular and ductal networks of the breasts are specialized variations of sweat glands and are actually organs of the skin rather than internal organs. The blood-flow and metabolic activity of the female breasts are highly influenced by estrogens and progesterone hormones and the phases of the menstrual cycle as well as pregnancy and lactation. These influences will manifest changes in the breasts' thermal features.
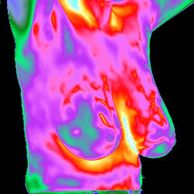
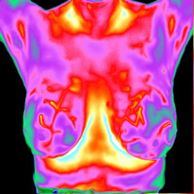
Typically, medical thermology indicates breast cancer by a detailed evaluation of the levels, patterns and behavior of “Hot Spots” on the skin that result from abnormal blood-flow and metabolic conditions characteristic of cancer. The “Hot Spots” of breast cancer occur as a result of the uncontrolled and excessive flow of the body's core-temperature blood to a relatively superficial area. This excessive blood-flow occurs simultaneously with the first cellular changes of cancer and precedes the development of a physically-discernible tumor. This explains the ability of medical thermology to provide the earliest objective indication of breast cancer, often years prior to structural-based diagnostic imaging, such as X-ray mammography and ultrasound.
Medical thermology cannot offer any reliable means to evaluate conditions involving the core (deep internal organs such as the heart, lungs, liver or kidneys) of the body as there is no means of directly affecting the skin's blood-flow.
The Short Answer: Most women should start annual breast thermology at 25 years of age and can be self-referred.
The Long Answer: Every expert agrees earlier detection of breast cancer enables earlier treatment with better results that saves lives. Breast thermology is completely safe (non X-ray) and often provides the very first objective indication for all forms of breast cancer and has a very high diagnostic sensitivity for women of all ages. Breast cancer is the largest cause of death for women aged 29-45 and, generally, breast cancer takes many years from its inception to the death of its victims. Therefore, most women would benefit by including breast thermology into their annual healthcare by the age of 25. Because the thermology imaging is without any risk of physical harm, women can be self-referred for routine screening. However, our laboratory requires every woman to share the breast thermology report with their professional healthcare provider that is capable of ordering the other indicated diagnostic procedures to complement her study. Breast thermology can also be useful to monitor changes to the specific metabolic and blood vessel features of breast cancer during and after many forms of treatment. However, this monitoring must be done in close coordination with the treatment program as directed by a personal physician.
The Short Answer: You will stand before the camera for two sets of images of your breasts from the front and the both sides with one-minute emersion of your hands in cool water between them.
The Long Answer: Please call our office for your appointment (Contact Us). A patient history form and pre-appointment instructions will be e-mailed to you. Please carefully read these instructions and fill out the online medical history form (including the name and mailing address of your personal physician(s)) before your appointment.
The thermology technologist will accompany you into the climate-controlled imaging room and review your completed history form. The thermology technologist will explain the full details of the imaging process and address your questions. You will be given privacy in a dressing area while you undress from the waist-up and keep your arms away from your body for approximately 15-20 minutes.
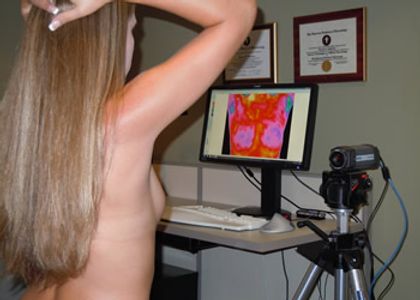
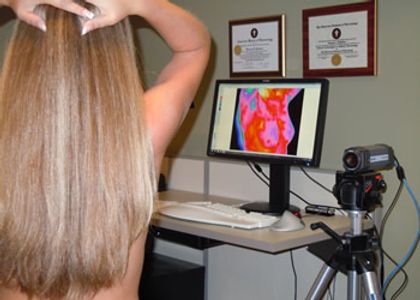
The thermology technologist will ask you to stand about four to six feet in front of the infrared camera and turn to your side while making the first image. Then you will be asked to turn to the opposite side for the second image and face directly into the camera for the third image.
You will be asked to place both hands into a basin of cool water for the autonomic challenge for one minute, quickly dry your hands and repeat the imaging sequence. You will be able to watch your own images on a video monitor as they are being recorded. Once the thermology technologist confirms the quality of your images, you may get fully dressed and leave.
The entire process is typically completed in thirty minutes from your appointment time. No objects, personnel, lights, nor any other forms of energy (non X-ray) are directed at you. Our clinic provides the highest standard of professionalism, respects your privacy and guards your confidential information under the HIPAA regulations.
Short Answer: NO!
The Long Answer: There can be many reasons for high thermal energy patterns (“Hot Spots”) in your breasts and cancer is only one of them. There is no distinct level or pattern of thermal energy that characterizes breast cancer and it is not "color-coded" on our video monitor. "Hot Spots" may be the result of tissue inflammation or other benign metabolic activity unrelated to cancer. The thermology technologist is not able to give you any immediate results based upon an impression of your images as the evaluation of your infrared images requires a specific, deliberate and detailed analysis with an objective and quantitative expert system before any conclusions are made.
Short Answer: Probably not. However, your cost is artificially low to make it affordable.
The Long Answer: There are established procedure (ICD-9) and insurance codes (CPT) for breast thermology but, currently, they are not payable by most insurers. This policy is attributable to the published results of obsolete studies, absence of comprehensive national standards for breast thermology and real issues of poor quality from some providers. Some medical health insurers do cover breast thermology on the written referral of your personal physician but others will contend "its value is unproven" or that "it is experimental". Neither of these statements are true as it has been demonstrated by the results of more than eight hundred articles published in major medical journals in the past fifty years and the statements of the US Food and Drug Administration, the National Cancer Institute and the Department of Health and Human Services. You may use funds from your Health Saving Account to pay for your breast thermology study and the cost is deductible as a legitimate health-related expense for your income taxes.
Short Answer: NO!
The Long Answer: There are certain specific diagnostic applications for thermology that are established by basic medical science and clinical experience. There is a respectable body of substantiating peer-reviewed clinical studies in the medical literature that is necessary for a legitimate diagnostic claim. Beyond this are some other applications that may be considered investigational when there is some level of basic medical science indicating the application and some objective clinical experience but then only in the context of an experiment. Some providers offer unsubstantiated diagnostic infrared imaging studies for “Visceral Health”, “Digestive Disorders: Irritable bowel syndrome, diverticulitis and Crohn’s disease”, “Immune Dysfunction”, “Nutritional disease (alcoholism, diabetes)”, “Chronic Fatigue” and “Gingivitis”. Thermology is not a legitimate diagnostic tool for every medical condition and we consider claims for these and other "whole body" studies to be speculative at best, irresponsible and probably a disservice to patients and Medicine. The FDA has cited some providers for unsubstantiated diagnostic claims (1, 2, 3). Therma-Scan has been at the forefront of innovation and development of medical thermology but we will not make diagnostic claims for novel applications without a solid basis in medical science and meaningful diagnostic parameters.
1. FDA Enforcement Actions/Warning Letter posted 22 March 2011
2. FDA Enforcement Actions/Warning Letter poster 04 April 2011
3. FDA Enforcement Actions/Warning Letter posted 17 April 2011
Short Answer: Not by itself.
The Long Answer: No single or even combined imaging tests can diagnose (definition: a medical conclusion) breast cancer. Cancer is diagnosed only by the most specific procedure possible; a detailed evaluation of an actual tissue sample (biopsy). Every form of medical imaging (X-ray mammogram, ultrasound, MRI and thermology) is intended to provide the specific characteristics of a disease (definition: diagnostic) that will indicate the individuals and exact locations that need to be biopsied.
All diagnostic tests are graded by their sensitivity (how well a test correctly identifies the presence of a disease) and specificity (how well a test correctly identifies the absence of a disease). Unfortunately, every means of diagnostic testing is imperfect and some are seriously degraded by patient conditions. Because of the high sensitivity (approximately 97%) and good specificity (approximately 75%) of breast thermology and given the risk level for breast cancer, we contend that every woman needs the combined benefits of several means of diagnostic imaging. Breast thermology is usually able to detect the earliest characteristic signs of breast cancer but is not able to provide the exact location of the abnormal cells with the precision necessary for a biopsy. Thus, a multi-modality program is necessary for the early detection of breast cancer. We contend that thermology is vital to the healthcare of every woman because of its high sensitivity and its complete safety.
Short Answer: Yes.
The Long Answer: No single means of testing for breast cancer is perfect or even sufficient. X-ray mammography’s sensitivity (how well a test correctly identifies the presence of a disease) is approximately 80% (misses 1 in 5 cancers) at best and has a practical detection threshold of tumors approximately 1 cm (a little less than ½ inch with about 4 million cells). The sensitivity of X-ray mammography is significantly degraded for pre-menopausal women, women with dense or fibrocystic breast tissue, women with implants, surgical reductions or prior biopsies, women with large or small breasts and with fast-growing cancer. X-ray mammography’s specificity (how well a test correctly identified the absence of a disease) is approximately 11% with a large number of false-positive errors. X-ray mammography is a structural study of the breasts that images details based on the differences in the tissues’ absorption of X-ray radiation. Usually this means the identification of clusters of small and irregularly shaped calcium deposits (micro-calcifications). Calcium deposits occur not just as a result of cancer but as a response to many forms of tissue stress. Calcium deposits are easily obscured by competing densities from glandular or scar tissue and some cancer grows too quickly to cause calcium deposits.
Breast thermology is not perfect either, but multiple clinical studies have established sensitivity (how well a test correctly identifies the presence of a disease) about 97% (misses about 3 in 100) and a specificity (how well a test correctly identifies the absence of a disease) of approximately 75%. Breast thermology indicates cancer by evaluating the specific levels, patterns and behavior of “Hot Spots” caused by abnormalities of blood-flow. There are very few conditions that can interfere with the sensitivity of breast thermology, but its specificity can be compromised by local sources of inflammation or other metabolic abnormalities. Thermology is effective for women with many of the conditions that degrade the effectiveness of X-ray mammography. Because the blood-flow changes characteristic of breast cancer usually occur years in advance of calcium deposits, thermology is able to indicate breast cancer before X-ray mammography. As the only means of objectively evaluating the functional disorders specific to breast cancer, we contend thermology has a vital role in every women's healthcare for breast cancer. However, abnormal thermology studies require some form of structural study (ultrasound, X-ray mammogram or MRI) to provide the specific site for a biopsy.
Short Answer: Medical thermology is available in a few major university-based medical centers. However, most hospitals have not determined any means by which to fund a thermology service or are satisfied with their existing imaging services.
The Long Answer: Most medical thermologists are specialists in neurology, surgery, vascular medicine or oncology that practice thermology as an adjunct within their specialty rather than as a discipline itself. There are very few trained and dedicated thermologists, not nearly enough to be available for even the major hospitals. The imaging services of most hospitals are run by radiologists and most radiologists have no useful abilities for thermology as it is based on medical function rather than medical structure. What little knowledge many radiologists have of thermology is outdated and they may be under peer-pressure to disregard thermology as an imaging system outside of their domain. Unfortunately, the current lack of effective national standards for quality and practices for thermology also acts to keep it out of the mainstream of Medicine.
Short Answer: Many physicians are uninformed or misinformed about medical thermology. Please ask your physician to read the Professionals section of this website or contact our office for a collection of published peer-reviewed scientific and medical studies.
The Long Answer: The rise in the incidence of breast cancer during the early 1970's and the early successes with medical infrared imaging generated a great deal of enthusiasm for it as a diagnostic tool. The early adopters of medical infrared imaging were able to demonstrate impressive sensitivity levels in their preliminary studies even using relatively primitive analog equipment and only a superficial level of empirical knowledge to guide their evaluations. In 1974, the US National Cancer Institute funded a large-scale study on the early detection of breast cancer as a means of reducing mortality and included medical infrared imaging almost as an afterthought and with some very poor planning. Unlike X-ray mammography, there were no specifications or standards for the equipment, technique, evaluation or reporting for medical infrared imaging in this study. In most instances, the investigators evaluating the patient studies had no meaningful training. The resulting failure of this study was widely misinterpreted as a failure of diagnostic infrared imaging - an impression that was often promulgated by other imaging specialists with professional and/or proprietary disinterests. The poor results from the Breast Cancer Detection and Demonstration Project effectively dampened the early enthusiasm for medical infrared imaging. However, medical scientists came to understand the fundamental basis for the "Hot Spots" of breast cancer and clinical studies developed an objective analytic system that lead to a major transformation from the empirical practices of thermography to the level of a proper (albeit young) science of thermology. Currently, there are more than 800 clinical studies involving more than 300,000 women that are published in peer-reviewed medical journals that validate the claims for early detection, very high sensitivity and good specificity of breast thermology. Unfortunately, it is very difficult to get a chance to change a first impression and many physicians hold outdated opinions without any real knowledge of the transforming developments for medical infrared imaging since the mid 1970's.
Short Answer: We are the most qualified and experienced facility that works to the highest standards of imaging, analysis and reporting.
The Long Answer: Therma-Scan is the premier source for medical thermology in the world. We earn our reputation for innovation, quality and integrity with every patient study. Therma-Scan is the most experienced and accomplished provider of medical-grade thermology in the world with more than one million patient studies since 1972. Therma-Scan uses the Marseille system “TH” scale in all of our breast thermology as a standardized reporting format that healthcare professionals can relate to the BI-RADS® system of X-ray mammography for improved patient care. We are the fountainhead of just about every quality development and practice in the field. Therma-Scan pioneered the development of truly quantitative analysis of patient studies and originated the “cold challenge” as a means of differentiating the characteristic abnormal behavior of breast cancer from benign “Hot Spots”. We are accredited by the only recognized, non-proprietary peer professional organization in North America; The American Board of Thermology. Our Laboratory Director is Board-Certified in Oncology, Vascular Medicine and Neuro-Science by the American Board of Thermology. Our laboratory has a five-stage quality control system to assure an unprecedented level of detail and excellence to every thermology report.
Above all, we are personally and professionally committed to provide the highest quality thermology study for each and every patient.
BI-RADS® is a registered trademark of The American College of Radiology
Copyright © 2011-2025 Therma-Scan™ Reference Laboratory, LLC - All Rights Reserved.
Images or text in this site may not be reproduced in part or whole in ANY format, electronic or printed without the expressed, prior and written approval of
Therma-Scan™ Reference Laboratory, LLC.
6239 E Brown Rd Suite #117
Mesa, AZ 85205
(602) 603-0749
Please like us on Facebook.
Therma-Scan™ Reference Laboratory, LLC. is a certified facility by the American Board of Thermology and the European Association of Thermology
Site Design by My Website Girl